What Is PAH Angiography and How Is the Procedure Performed?
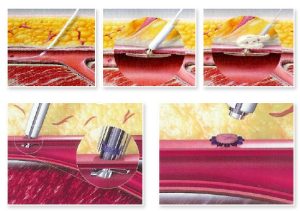
Pulmonary arterial hypertension (PAH) angiography is a specialized diagnostic technique that provides a direct, high-resolution view of the pulmonary arteries to assess pressure, flow, and structural abnormalities within the lung circulation. During this minimally invasive procedure, an interventional cardiologist or radiologist introduces a thin, flexible catheter—typically through the femoral vein in the groin or the internal jugular vein in the neck—and gently advances it under X-ray guidance into the right side of the heart and then into the pulmonary artery. Once the catheter tip is positioned within the main pulmonary artery, contrast dye is injected to outline the arterial branches on real-time fluoroscopy. This allows the care team to measure pulmonary artery pressures, evaluate the presence of narrowing or obstructions, and detect vascular remodeling characteristic of PAH. Throughout the procedure, continuous hemodynamic monitoring ensures patient safety as we record pressure readings, oxygen saturations, and cardiac output. After completing angiographic imaging, the catheter is withdrawn, and a small pressure seal or closure device is applied to the vascular entry site. Most patients spend only a few hours under observation before returning home the same day or the following morning, depending on individual risk factors and response. We provide seamless coordination of imaging, sedation, and follow-up care to ensure that every aspect of your PAH angiography experience is handled with precision and compassion—contact us for more details on how we perform this critical assessment with cutting-edge technology and expert guidance.
Who Is an Ideal Candidate for Pulmonary Arterial Hypertension Angiography?
Determining candidacy for PAH angiography begins with a thorough evaluation by a pulmonary hypertension specialist, typically involving clinical assessment, echocardiography, exercise testing, and advanced imaging such as CT pulmonary angiography. Patients exhibiting unexplained shortness of breath, fatigue, chest discomfort, or syncope on minimal exertion—especially when initial noninvasive tests suggest elevated pulmonary pressures—stand to benefit most from invasive confirmation via angiography. Ideal candidates include individuals with suspected idiopathic PAH, those with systemic sclerosis or connective tissue diseases at high risk for pulmonary vascular involvement, and patients with congenital heart disease who demonstrate right ventricular enlargement or unexplained hypoxemia. Angiography also plays a vital role in differentiating PAH from other forms of pulmonary hypertension—such as chronic thromboembolic pulmonary hypertension (CTEPH)—by visualizing organized thrombus and vascular webs that may require distinct therapies like pulmonary thromboendarterectomy. Additionally, PAH angiography informs treatment planning for patients being considered for advanced therapies, including prostacyclin analog infusions, endothelin receptor antagonists, and phosphodiesterase-5 inhibitors, by providing precise hemodynamic data and vascular mapping. Before recommending angiography, we carefully review each patient’s overall health, coagulation status, and renal function to minimize procedural risks. If you or a loved one have symptoms or risk factors for pulmonary hypertension that warrant definitive evaluation, reach out to schedule a consultation—our multidisciplinary team will guide you through candidacy assessment and deliver personalized recommendations every step of the way.

What Are the Risks and Side Effects of PAH Angiography?
While PAH angiography is generally safe when performed by experienced interventional specialists, it carries inherent risks that we manage proactively through meticulous pre- and intra-procedural care. The most common side effects include mild discomfort or bruising at the vascular access site, transient itching or warmth as the contrast dye circulates, and a brief sensation of flushing. Less frequently, patients may experience arrhythmias—such as premature ventricular contractions or transient heart block—when the catheter passes through the right heart chambers; we monitor cardiac rhythm continuously and can administer medications or temporarily reposition the catheter to resolve these events. Contrast-induced kidney injury, particularly in patients with pre-existing renal impairment, is another consideration; we mitigate this risk by ensuring adequate hydration, using low-osmolar contrast agents, and carefully calculating dye volume. Rare but serious complications include arterial dissection, pulmonary artery perforation, or major bleeding at the access site; in such cases, our interventional team is fully equipped to provide immediate endovascular repair or surgical intervention if necessary. We also take universal precautions to prevent infection, administering prophylactic antibiotics when indicated and employing sterile techniques throughout. A thorough review of your medical history and tailored risk assessment allow us to optimize safety and minimize potential side effects. Throughout your PAH angiography journey, our dedicated care coordinators remain available to address any concerns, ensuring that you receive prompt attention and reassurance at every turn—contact us to learn more about how we prioritize your safety and comfort.
How Should You Prepare for a PAH Angiography Appointment?
Optimal preparation for PAH angiography involves both medical and logistical steps to ensure your comfort and the accuracy of your results. In the days before your appointment, you will undergo baseline laboratory tests—including complete blood count, kidney and liver function panels, coagulation studies, and allergy screening for contrast agents—as well as a thorough clinical review of your current medications. We advise holding certain blood thinners or antiplatelet drugs according to a schedule determined by your cardiologist, while continuing essential heart or blood pressure medications unless otherwise instructed. You may be asked to fast for six to eight hours before the procedure to reduce aspiration risk during sedation. Plan to arrive at our center with a responsible adult companion, as you will require assistance to travel home safely afterward. Wear comfortable clothing with easy access to your groin or neck area, depending on your access site, and bring a comprehensive list of your current medications and any relevant medical records. Our team will provide clear guidelines on hydration, pre-procedure fasting, and checkpoint times; we’ll also review sedation options and address any anxieties you may have. On the day of angiography, a nurse will place an intravenous line, perform vital sign checks, and review consent forms to ensure all your questions are answered. By following these preparation steps, you help us deliver precise diagnostic information in a comfortable, stress-free environment—reach out for your personalized pre-angiography checklist and let us guide you through each preparatory milestone.
What to Expect During a Pulmonary Hypertension Angiogram
The experience of a pulmonary hypertension angiogram unfolds in a series of well-orchestrated phases designed for both safety and customer comfort. Upon arrival, you will be welcomed by our specialized nursing staff who will escort you to a private prep area where your vital signs are recorded and sedation options are discussed. Conscious sedation—typically a combination of midazolam and fentanyl—helps you remain calm and comfortable, while local anesthesia numbs the access site. In the angiography suite, you lie supine on a radiolucent table, and a state-of-the-art fluoroscopy system allows real-time visualization of catheter movement. Under sterile conditions, the interventionalist introduces the catheter through the femoral or jugular vein and gently advances it into the right atrium, right ventricle, and subsequently the main pulmonary artery. As the catheter reaches each chamber, pressure measurements and blood samples are obtained to calculate pulmonary vascular resistance and cardiac output. At the pulmonary artery, a contrast injection illuminates the vascular tree, enabling delineation of any stenoses, webs, or aneurysms. The entire catheterization and imaging sequence lasts between 45 and 90 minutes. Once complete, the catheter is withdrawn, and a vascular closure device or manual pressure is applied to secure hemostasis. You will then rest in our recovery area, where nurses monitor your vital signs, perform puncture site checks, and gradually wean sedation. Most patients experience minimal discomfort throughout and can expect to remain under observation for two to six hours before discharge with post-procedure care instructions. Our multidisciplinary team remains on call to answer any questions during your recovery at home—contact us to learn how we ensure a smooth, informative, and reassuring angiography experience.
How Long Is the Recovery Time After PAH Angiography?
Recovery from pulmonary arterial hypertension (PAH) angiography is generally rapid and well tolerated, reflecting the minimally invasive nature of the catheter-based procedure. Most patients spend just a few hours under observation in a recovery area, during which nursing staff monitor vital signs, inspect the vascular access site for bleeding or bruising, and ensure that sedation effects have sufficiently worn off. While individual experiences vary, many people feel comfortable enough to return home the same day once their blood pressure, heart rate, and oxygen saturation remain stable and they can ambulate safely without significant dizziness or pain. Mild groin soreness or bruising at the catheter insertion site may persist for several days, but any discomfort is typically managed with over-the-counter analgesics and detailed home-care instructions we provide. Patients are advised to avoid strenuous activity, heavy lifting, and prolonged standing for 24 to 48 hours to reduce the risk of bleeding, but most resume light daily tasks the very next day. Formal exercise—such as brisk walking or gentle cycling—can often restart after two to three days, while more vigorous workouts like running or weightlifting are usually deferred for one to two weeks. Throughout this period, our team schedules follow-up calls or visits to address any emerging questions, assess healing, and review your hemodynamic results. By coordinating each step of your post-procedure journey and providing clear recovery guidelines, we help you return to normal life quickly, safely, and with confidence in your cardiovascular health.
PAH Angiography Cost: Is It Covered by Insurance?
Understanding the financial aspects of PAH angiography is crucial for planning and peace of mind, and coverage varies across countries and insurance plans. In many healthcare systems, right heart catheterization with pulmonary angiography—often billed under cardiac catheterization or interventional cardiology procedures—qualifies as a medically necessary diagnostic test for suspected pulmonary hypertension, making it eligible for reimbursement under most major public and private insurance schemes. The total cost typically includes facility and equipment fees, professional fees for the interventionalist and anesthesiologist, imaging contrast materials, monitoring, and post-procedure observation. We provide a transparent, itemized estimate up front, so you understand each component of your bill. Our financial coordinators liaise directly with insurers to confirm coverage details, submit pre-authorization requests, and clarify any co-pay or deductible requirements. For international patients seeking evaluation in Turkey’s accredited centers, we offer comprehensive medical tourism packages that bundle the angiography itself with pre-procedure testing, accommodation, transportation, and follow-up visits at a discounted rate—enabling you to concentrate on your health rather than logistics. If your insurance plan requires partial out-of-pocket payment, we facilitate flexible payment plans to spread costs over several months. Contact us for a personalized cost review and insurance consultation, and we will work tirelessly to maximize your benefits and minimize unexpected expenses.
Right Heart Catheterization vs. PAH Angiography: What’s the Difference?
Right heart catheterization and PAH angiography share many procedural elements but serve complementary diagnostic roles in evaluating pulmonary vascular disease. Right heart catheterization measures static and dynamic hemodynamic parameters—mean pulmonary artery pressure, pulmonary capillary wedge pressure, cardiac output, and pulmonary vascular resistance—without necessarily visualizing the pulmonary arterial tree in detail. PAH angiography, by contrast, incorporates selective contrast injections into the pulmonary arteries to provide high-resolution imaging of vessel anatomy, detect web-like lesions, small branch stenoses, or thromboembolic obstructions that might not be apparent on hemodynamic data alone. In practice, we perform right heart catheterization first to confirm elevated pulmonary pressures and calculate resistance indices; if vascular remodeling or obstruction is suspected, we extend the procedure to include angiographic runs. This dual approach ensures that both functional and structural aspects of the pulmonary circulation are assessed during a single catheterization session, sparing you a second invasive test. Modern interventional suites seamlessly integrate pressure transducers and digital subtraction angiography, allowing us to switch between pressure measurements and imaging with minimal catheter manipulation. By combining these techniques—right heart catheterization for precise hemodynamics and PAH angiography for detailed mapping of arterial lesions—we deliver a comprehensive cardiovascular assessment in one efficient procedure. Reach out to learn how we tailor this integrated approach for your unique clinical needs.
Can PAH Angiography Detect All Forms of Pulmonary Hypertension?
PAH angiography excels at diagnosing pulmonary arterial hypertension (WHO Group 1) and chronic thromboembolic pulmonary hypertension (CTEPH, WHO Group 4) by visualizing narrowed, tortuous, or obstructed arterial segments and measuring the downstream pressure impact. However, not every form of pulmonary hypertension is best assessed by angiography alone. Pulmonary hypertension due to left heart disease (Group 2) often results from elevated left atrial pressures and pulmonary venous congestion, which require echocardiography, left heart catheterization, and ventilatory assessments to distinguish. Similarly, pulmonary hypertension associated with lung diseases like chronic obstructive pulmonary disease and interstitial lung disease (Group 3) manifests predominantly through parenchymal changes and hypoxic vasoconstriction; high-resolution CT scans and pulmonary function tests are the mainstays for these categories. While PAH angiography can provide supportive information in these contexts—such as excluding concurrent arterial obstructions—it cannot replace the comprehensive imaging and functional studies needed to classify non-arterial forms of pulmonary hypertension accurately. In our multidisciplinary pulmonary hypertension program, we integrate angiographic findings with echocardiography, high-resolution CT, ventilation-perfusion scans, and cardiopulmonary exercise testing to ensure that every subtype of pulmonary hypertension is correctly diagnosed and managed. Whether you require arterial mapping for PAH or a broader diagnostic workup for lung disease–related hypertension, our coordinated team will guide you through the optimal sequence of noninvasive and invasive studies.
Non-Invasive Alternatives to PAH Angiography
For patients in whom invasive procedures pose excessive risk or who prefer to defer catheterization, several non-invasive modalities offer valuable insights into pulmonary pressures and right heart function. Doppler echocardiography estimates pulmonary artery systolic pressure by measuring tricuspid regurgitant jet velocity and assessing right ventricular size and function; while less precise than direct catheter measurements, echocardiography serves as a useful screening and monitoring tool. Cardiac magnetic resonance imaging (MRI) provides detailed assessment of right ventricular volumetrics, myocardial fibrosis, and relative blood flow in the pulmonary arteries, low radiation exposure, and unrivaled soft-tissue contrast. Ventilation-perfusion (V/Q) scanning excels at detecting chronic thromboembolic pulmonary hypertension by demonstrating mismatched perfusion defects. Advanced computed tomography (CT) pulmonary angiography, with high-resolution 3D reconstructions, visualizes arterial webs, stenoses, and vessel pruning suggestive of PAH or CTEPH. Finally, cardiopulmonary exercise testing (CPET) evaluates exercise-induced pulmonary hypertension by measuring oxygen consumption, ventilation, and hemodynamics during graded exertion. While none of these techniques provide the definitive pressure readings that only catheterization can offer, they collectively reduce the reliance on invasive angiography in certain clinical scenarios. Our center leverages these non-invasive tools for early detection, follow-up assessment, and risk stratification—ensuring that invasive angiography is reserved for patients most likely to benefit from direct hemodynamic and anatomical evaluation. Contact us to explore how a tailored non-invasive diagnostic pathway can deliver the information you need while minimizing procedural risks.
How to Read and Understand Your PAH Angiography Results
Interpreting the detailed data from a pulmonary arterial hypertension (PAH) angiogram can feel overwhelming, but understanding key parameters empowers you to participate actively in your care. Your angiography report will typically include measurements of mean pulmonary artery pressure (mPAP), pulmonary capillary wedge pressure (PCWP), cardiac output (CO), and pulmonary vascular resistance (PVR). An mPAP above 25 mm Hg at rest confirms pulmonary hypertension, while a normal PCWP (below 15 mm Hg) helps distinguish PAH (pre-capillary) from heart failure–related pulmonary venous hypertension (post-capillary). Cardiac output—often calculated by the Fick method or thermodilution—reveals how effectively your right ventricle pumps blood into the lungs, and an elevated PVR (above 3 Wood units) indicates increased resistance downstream in the small pulmonary arteries.
Beyond these numbers, angiographic images reveal the anatomical landscape: look for areas of vessel narrowing, pruning of peripheral branches, or evidence of small web-like obstructions that may suggest chronic thromboembolic disease. Your physician will review each image with you, pointing out any regions where contrast flow slows or diverts, and correlating these findings with pressure data to form a comprehensive picture of your pulmonary vascular health. We provide annotated copies of your angiogram films and easy-to-follow summaries of your hemodynamic data—reach out if you’d like a personal walkthrough of your results, complete with visual aids and plain-language explanations that clarify what each value means for your treatment plan.
Accuracy of PAH Angiography for Diagnosing Pulmonary Arterial Hypertension
Right heart catheterization with angiographic mapping remains the gold standard for diagnosing PAH, offering unmatched precision compared to non-invasive tests. While echocardiography estimates pressures indirectly and CT or MRI visualizes structure, only catheter-based angiography directly measures real-time pressures and resistance while simultaneously highlighting anatomical lesions. Studies demonstrate that catheter-derived mPAP measurements have less than 5 percent variability when repeated under the same conditions, and pressure gradients recorded across arterial segments accurately pinpoint localized obstructions with over 90 percent sensitivity. The combination of functional and structural data in a single procedure reduces misclassification, ensuring that patients whose disease might be missed by non-invasive screening are identified promptly. By unifying hemodynamic precision with high-resolution vascular imaging, PAH angiography arms your care team with the definitive information needed to select targeted therapies—whether prostacyclin analogs, endothelin receptor antagonists, or surgical options for chronic thromboembolic pulmonary hypertension. Contact us to learn how our state-of-the-art angiography lab maintains rigorous quality controls and employs advanced pressure transducers and digital subtraction angiography to maximize diagnostic accuracy.
Is PAH Angiography Safe During Pregnancy?
Pregnancy introduces unique considerations for women with suspected pulmonary hypertension, as both maternal and fetal health depend on accurate assessment and management. Although right heart catheterization carries radiation exposure concerns, modern angiography suites use low-dose fluoroscopy protocols, abdominal shielding, and pulsed imaging to minimize fetal dose—often keeping it well below established safety thresholds. Conscious sedation agents like midazolam and fentanyl have favorable safety profiles in pregnancy when used in controlled, single-dose settings. Extensive registries indicate that, with meticulous technique and multidisciplinary oversight by maternal-fetal medicine specialists and cardiologists, the procedural complication rate remains comparable to non-pregnant cohorts, and the benefits of definitive hemodynamic data typically outweigh the small radiation risks.
For women in their second trimester—the period of organ maturation and relative hemodynamic stability—angiography safely informs decisions regarding vasodilator therapy, delivery planning, and anticoagulation if needed. Pre-procedure collaboration among obstetrics, anesthesia, and interventional cardiology ensures that maternal positioning avoids compression of the inferior vena cava, while continuous fetal monitoring provides reassurance throughout. If pulmonary hypertension is severe, timely angiographic confirmation can be lifesaving, guiding the initiation of targeted medications that improve cardiac output and uteroplacental perfusion. We offer dedicated pregnancy-safe angiography pathways, complete with patient education, individualized risk–benefit discussions, and specialized nursing support—reach out to explore how we balance precise diagnosis with maternal and fetal well-being.
Tips to Manage Anxiety Before Your PAH Angiography
Feeling apprehensive before a catheter-based procedure is perfectly natural, and we believe in equipping you with strategies to manage anxiety and approach your angiogram with calm confidence. First, schedule a pre-procedure visit or virtual tour of our angiography suite, so the environment and team members become familiar; knowing what to expect greatly reduces fear of the unknown. Practice guided breathing exercises—such as inhaling deeply for four counts, holding for two, and exhaling for six—to activate your parasympathetic system and lower heart rate prior to sedation. Listening to soothing music or using noise-canceling headphones during preparation can create a comforting auditory cocoon.
Discuss sedation options openly with your physician: mild anxiolytics like low-dose benzodiazepines administered prior to the procedure can ease nerves without impairing recovery. Cognitive reframing techniques—viewing the angiogram as an empowering diagnostic step toward better health rather than a threatening intervention—shift your mindset from fear to hope. Enlist a support person to accompany you on the day, providing emotional grounding and practical assistance. Finally, address any lingering questions head-on: whether about radiation levels, catheter sensations, or post-procedure recovery, clarity fosters trust and diminishes anxiety. We prioritize personalized pre-procedure counseling, offering one-on-one sessions with our interventional team to walk you through each phase and ensure your concerns are fully addressed—contact us to arrange a dedicated anxiety-management consultation and transform apprehension into assurance.

